
The American Association of Post-Acute Care Nursing (AAPACN) recently hosted the AAPACN 2023 Quality Virtual Conference, a one-day virtual conference that brought together leaders and experts in quality improvement to provide attendees with the information and resources necessary to monitor quality measures and outcomes for improved performance for both skilled nursing facilities (SNFs) and home health agencies (HHAs). For those unable to attend the event on June 14, AAPACN is offering a bundle of the sessions for on-demand learning. Learn more here.
In conjunction with that event, AAPACN asked attendees to submit their questions on Quality Measures (QMs) from any program—MDS 3.0 QMs, Quality Reporting Program (QRP) QMs, Value-Based Purchasing QMs, those that impact Five-Star, or those publicly reported on Nursing Home Compare—to the AAPACN Leading in Care Blog. Below are the responses to their questions.
Question 1: This question is related to the Value-Based Purchasing (VBP) report. I would like to know how each resident triggers and why.
Response from Jessie McGill, RN, BSN, RAC-MT, RAC-MTA, AAPACN Curriculum Development Specialist:
The Skilled Nursing Facility (SNF) Value-Based Purchasing (VBP) program currently uses only one readmission measure—the SNF 30-Day All-Cause Readmission Measure (SNFRM). However, the VBP program will soon expand to include more measures starting in FY 2026. The SNF VBP Confidential feedback report will show your eligible stays, number of readmissions that qualified for the measure numerator, and the standardized readmission rate. This measure also uses two years of Medicare claims data to determine if a resident triggers. Here are the periods used for FY 2023 and FY 2024:
- FY 2023:
- FY 2019 (10/1/2018–9/30/2019) FY 2021 (10/1/2020–9/30/2021)
- FY 2024
- FY 2019 (10/1/2018–9/30/2019) FY 2022 (10/1/2021–9/30/2022)
To answer your question in simple terms, any resident who admits directly from the hospital to start a Medicare Part A stay and is readmitted back to the hospital for an unplanned inpatient stay within 30 days of discharge from the hospital will trigger for this measure, unless an exclusion was met. This measure only uses Medicare claims data to calculate discharges from the hospital, SNF admissions, and readmissions to the hospital. No MDS data is used for this measure.
To provide a bit more technical detail, a resident will trigger the SNFRM if they are a Medicare Part A beneficiary who was admitted to a SNF within one day of discharge from an inpatient stay at a Medicare-participating hospital and has an unplanned hospital inpatient readmission within 30 days of the hospital discharge. However, there are exclusions: admissions to other PAC settings, a gap in stay between hospital and SNF, less than 12 months of Medicare enrollment, discharging against medical advice, cancer treatment, prostheses or pregnancy-related hospitalizations, and stays from a critical access hospital. More detailed information is available in the SNFRM Technical Report.
Question 2: On the SNF QRP review and correct reports, how can you tell why a resident is flagging for the discharge self-care and/or mobility report when some of it is related to the comorbidities? We have some residents who gained quite a bit and on discharge still end up flagging.
Response from Jessie McGill, RN, BSN, RAC-MT, RAC-MTA, AAPACN Curriculum Development Specialist:
This is a great question that does not have a great answer. The Discharge Function measures, for both self-care and mobility, use a calculated expected discharge score for each stay. This is a very complex statistical calculation that is not made available in any of the reports. In this year’s proposed rule comments period, AAPACN asked the Centers for Medicare & Medicaid Services (CMS) to include the calculated observed and expected scores for discharge so that providers can see how close they were to achieving goals and where to focus improvement efforts. On the resident level SNF QRP report, the discharge scores are only displayed as a desirable outcome (“x” indicates resident met the discharge expected score, NT (bolded) indicates resident did not meet the desirable outcome of meeting the discharge expected score). Since the expected discharge score is displayed this way, there is no possible way to see how close the resident was to meeting the expected discharge score or how the resident’s risk-factors or comorbidities affected the score.
The expected discharge score is also not something that can be calculated by the SNF – the SNF QRP Program Measure Calculations and Reporting User’s Manual, v4.0, provides this formula:

So, while you may have had a resident make strong gains or even meet discharge goals, if the resident did not meet or exceed the expected discharge score, the resident will count against this measure.
Question 3: How long do facility-acquired pressure injuries stay on your quality measures?
Response from Jennifer LaBay, RN, RAC-MT, RAC-MTA, QCP, CRC, AAPACN Curriculum Development Specialist:
The long stay measure, Percent of High-Risk Residents With Pressure Ulcers, uses target assessment methodology for calculation. The target assessment is the most recent assessment submitted within the target period, which is three months for long-stay measures. This QM will trigger when a resident has a high-risk pressure ulcer Stage 2-4, regardless of whether it was facility acquired or not—but keep in mind, this measure only includes residents who have been in your facility for 101 days or more. The resident will continue to trigger until an assessment that does not have a high-risk Stage 2-4 or unstageable pressure ulcer coded on the target assessment. Residents are considered high-risk and included in the denominator if they have one of the following: impaired bed mobility or transfer, comatose, or a diagnosis of malnutrition (or risk of malnutrition). More information on when a QM triggers can be found in the new AAPACN tool, When MDS 3.0 Quality Measure Triggers Start and Stop.
The short stay measure, Changes in Skin Integrity Post-Acute Care: Pressure Ulcer/Injury, uses the SNF Quality Reporting Program (QRP) QM and calculates the number of Medicare Part A SNF stays in the 12-month target period, during which a resident had a facility-acquired or worsened Stage 2-4 or unstageable pressure ulcer/injury. This is calculated on the discharge assessment by subtracting the number of pressure ulcers/injuries that were present on admission, from the total number present for each stage and unstageable (M0300B-G). Since residents can only trigger on the discharge assessment, only “Type 1 SNF Stays” are included, which means the stay must have a paired 5-Day and discharge assessment. Residents who expired during the stay (Type 2 SNF stays) are excluded. If the resident’s stay triggered this measure, it will continue to trigger until the resident’s stay is no longer in the 12-month target period.
Question 4: Where does the Five-Star Quality Measures data come from and what time periods are used?
Response from Jessie McGill, RN, BSN, RAC-MT, RAC-MTA, AAPACN Curriculum Development Specialist:
The Five-Star Quality Rating System uses a complex methodology that is detailed in the Design for Care Compare Nursing Home Five-Star Quality Rating System: Technical Users’ Guide, most recently updated in January 2023. This manual provides information on the MDS- and claims-based measures used, minimums required, and how missing data is handled. Additionally, the manual explains that the data used for Five-Star QMs is from the last four full quarters and is updated quarterly. However, it’s important to recognize that there is a delay, which allows providers to review and correct information after it is submitted, but before it is used for public reporting. Once publicly reported, changes to the source MDS data will not change the public data.
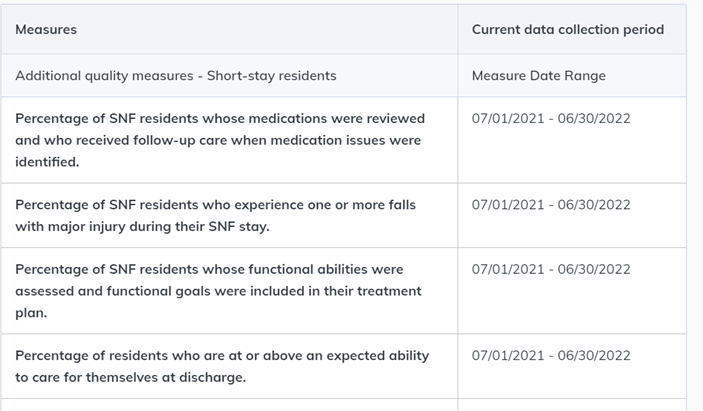
The Care Compare website includes a helpful resource. Once a facility is selected, and you have drilled into the Quality Measure domain, there is a link to “Get current data collection period.” This link will detail, for each measure, the exact time period of data that is being publicly reported and used in the Five-Star QM Rating domain.
Question 5: For Nursing Home Compare claims-based measures:
- What are the periods that are going to be reported on and how often does this change?
- Who is included and excluded from claims-based measure data?
Response from Jessie McGill, RN, BSN, RAC-MT, RAC-MTA, AAPACN Curriculum Development Specialist:
- The Nursing Home Compare (NHC) claims-based measures use a 12-month period of data and are updated quarterly. However, there is a lag time of six months, so that the data used is from stays 6-18 months ago.
- The NHC claims-based measures also have many exclusions, most of which are from fee-for-service (FFS) Medicare claims and/or Medicare enrollment data, as well as MDS data. For details on the exclusions for each measure, see the Nursing Home Compare Claims-Based Quality Measure Technical Specifications (March 2023), in the Downloads section of the CMS Quality Measure webpage and located in the MDS_QM_Users_Manual_V15_Update_03-22-2023 ZIP file.
Question 6: Can “Locomotion on unit” be captured for residents who move around in their room, but do not leave their room during the look-back period?
Response from Jessie McGill, RN, BSN, RAC-MT, RAC-MTA, AAPACN Curriculum Development Specialist:
Yes, the direct care staff should include walking or using a wheelchair while in the room under locomotion on unit. The definition of locomotion on unit in the RAI User’s Manual is, “How resident moves between locations in his/her room and adjacent corridor on same floor. If in a wheelchair, self-sufficiency once in chair.” This definition does not require that the resident also have locomotion in the adjacent corridor, so if only “in room” locomotion occurs, this would be used for MDS coding. If the resident has locomotion in room and also in the adjacent corridor, then the resident’s performance in both areas would be considered.

