The Activities of Daily Living (ADLs) in section G of the MDS are interwoven throughout the Care Area Assessments (CAAs), Quality Measures (QMs), and some state Medicaid reimbursement systems—and have been for years. Yet CMS took nurse assessment coordinators (NACs) by surprise when the draft MDS item sets released in early January 2020 revealed that section G would be removed from all OBRA and PPS assessments. That removal was postponed due to stakeholder concerns and the COVID-19 public health emergency, yet CMS has re-announced section G’s removal from the comprehensive OBRA item set starting October 1, 2023, and has released a draft MDS Nursing Home Comprehensive (NC) Item Set, v.1.18.11 reflecting that change.
Today, facilities must confront section G’s future removal, a development that raises more questions than answers. Many NACs are asking what effect the removal will have on the accuracy of the functional data collected, which in turn affects CAAs, care plans, QMs, and possibly even Medicaid reimbursement. While the details of the transition are not yet known, we can identify expected impact on different items and programs. This article will explore those potential impacts and how facilities can prepare for this change.
How will section GG replace section G?
On the draft item set, new instructions have been added for the assessment period for an OBRA admission, OBRA discharge, and OBRA assessments during the stay:
- On Admission:
- Assessment period is the first three days of the stay.
- Complete if A0310A = 01 [Admission assessment].
- If A0310B = 01 [PPS 5-Day scheduled assessment], the stay begins on A2400B [Medicare start date] and both columns [1. Admission performance and 2. Discharge goal] are required. If A0310B = 99 [Not PPS Assessment, None of the above], the stay begins on A1600 [Entry date] and only column 1 is required.
- On Discharge:
- Assessment period is the last three days of the stay.
- Complete only if A0310F = 10 or 11 [OBRA Discharge assessments] or A0310H = 1 [PPS Discharge assessment].
- If A0310G is not = 2 [Unplanned discharge] and A0310H = 1 [PPS Discharge assessment] and A2400C [Medicare end date] minus A2400B [Medicare start date] is greater than 2 and A2105 is not = 04 [Discharge status to short-term general hospital], the stay ends on A2400C [End date of most recent Medicare stay]. For all other Discharge assessments, the stay ends on A2000 [discharge date].
- During the stay
- Assessment period is the [assessment reference date] ARD plus two previous calendar days
- Complete only if A0310A = 02 – 06 [02. Quarterly review assessment, 03. Annual assessment, 04. Significant change in status assessment, 05. Significant correction to prior comprehensive assessment, or 06. Significant correction or prior quarterly assessment] and A0310B = 99 [Not a PPS assessment, None of the above], or A0310B = 08 [IPA – Interim Payment Assessment].
Essentially, the section GG performance period is a 3-day assessment period of the resident’s usual performance. On admission, if there is no 5-Day PPS assessment attached, the 3-day assessment period is the date of entry into the facility (A1600) and the two following calendar days. For an OBRA Discharge assessment that is not combined with a PPS Discharge assessment, the assessment period is the date of discharge (A2000) and the two previous calendar days. All other OBRA assessments and the interim payment assessment (IPA) will use the date of the ARD and two previous calendar days. If an OBRA assessment is combined with a PPS assessment, use the assessment period indicated with the PPS assessment instructions. The only other coding instruction on the draft item set is to “Code the resident’s usual performance for each activity using the 6-point scale. If an activity was not attempted, code the reason.”
While CMS has not yet posted an updated RAI User’s Manual to provide the full coding instructions, there is an indication of the future regarding the collection of functional data on OBRA Admissions, Quarterlies, Annuals, Significant Change in Status Assessments (SCSAs), and Significant Correction Assessments using the new 3-day lookback for Functional Abilities.
The removal of section G will cause a ripple effect of changes due to how frequently the ADLs were incorporated into other processes and programs, from the care areas to the QMs.
Care Area Assessment (CAA) and Care Planning

Of the 20 care areas, 17 (see chart on the right) currently use section G ADLs as care area triggers or as considerations on the Appendix C CAA worksheets. This means that when section G is removed from the item set, CMS will need to update the care area logic triggers and worksheet considerations. Many software companies have integrated the care area triggers and the Appendix C Review of Indicators worksheets into the MDS software. Providers should work with their software vendors to understand the changes that will be incorporated into their programs and coordinate training as needed.
Care plans may also have goals that are specific to section G or how the ADLs are currently coded. For example, if Mr. G has a goal to complete certain ADL tasks with limited assist, this may need to be documented differently to allow for a measurable goal beyond this transition. In section GG, function assist that requires non-weightbearing assistance falls under code 04, Supervision or touching assist. So, the “limited assist” goal may need to be updated to something like “touching/steadying and/or contact guard assistance” to better align with how this task will be coded under section GG.
Quality Measures
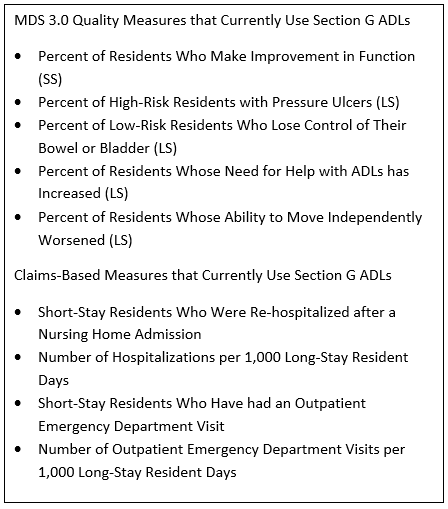
Currently, skilled nursing facilities (SNFs) monitor several different quality initiative programs, including MDS 3.0 Quality Measures, Nursing Home Compare Claims-Based Measures, Five-Star Quality Measures, SNF Quality Reporting Program (QRP) Measures, and the SNF Value-Based Purchasing (VBP) Measure. The MDS-based measures use MDS data for the numerator, denominator, risk-adjusting covariates, or exclusion factors. Many of the claims-based measures also utilize the MDS data in the risk-adjusting covariates.
There may be a delay between data collection and CASPER report availability, and an even longer delay for public reporting on Care Compare. This will result in a transition period between the retirement of section G ADL data (anticipated September 30, 2023) and the collection of section GG data, where the publicly reported data will continue to be displayed as ADL data. There may also be delays in when the MDS 3.0 Quality Measure Technical User’s Guide and the Nursing Home Compare Claims-Based Quality Measure Technical Specifications will be updated to reflect the removal of section G and possible remapping to section GG data.
Medicaid Case-Mix Reimbursement
Another looming question is how states that currently use section G ADLs as part of their case-mix Medicaid reimbursement methodology will adapt to the removal of section G. While a handful of states have already started a transition to a PDPM-based payment model, many case-mix states continue to use previous payment models, such as RUG-IV, RUG-III, a hybrid RUGs model, or another standard payment model.
Each state Medicaid program can establish its payment methodology, which may result in widely varying changes throughout the Medicaid case-mix states. It will be important for SNFs to establish a line of communication with their state’s Medicaid department to ensure understanding and a smooth transition because of the potential impact on revenue.
How to start preparing
- Care plan goals can be updated and reviewed now. When completing Annual assessments or Significant Change in Status Assessments (SCSAs), review all functional goals. Update the goals so they can be measured using either section G, ADL data, or section GG, Functional Abilities.
- For example, instead of having a goal to complete a task with “limited assist,” use descriptive words, such as “non-weight bearing assist” or “contact-guard assist.” These terms can be measured using either section G or GG data.
- Open a line of communication with the state Medicaid department. They may not have answers yet, but the team can find out how communication will be made available to SNFs with this proactive approach.
- Education for nurse aides will need to wait until more information is made available.
- First, you will need to know definitively what methodology your state Medicaid payment model is going to use. In addition, if your state is going to use GG, section G will continue to be coded through your state’s transition date—so education must be planned accordingly to prevent confusion and inaccurate coding.
- Second, CMS has not yet released the revised RAI User’s Manual, which will contain the full coding instructions vital for accurate coding.
- Keep up with MDS-related news. Nurse leadership (especially nursing home administrators and directors of nursing services) and NACs should stay abreast of MDS-related news to ensure timely planning and education.
- Follow AAPACN’s Post-Acute Care News (available to members)
- Look out for upcoming emails, webinars, podcasts, and articles from AAPACN on the changes.
- Check CMS’s Minimum Data Set (MDS) 3.0 Resident Assessment Instrument (RAI) Manual webpage regularly.
For permission to use or reproduce this article in full or in part, please complete a permissions form.
