Imagine sitting in a quality assurance and performance improvement (QAPI) meeting while different team members take turns reporting count data or the number of occurrences of an issue in the month. For example, the director of nursing services (DNS) might share two residents had unplanned weight changes, 10 falls happened, and five in-house acquired pressure injuries occurred in January. After the DNS finishes reporting, another leader shares that department’s count data. Throughout this meeting, you and other team members may be wondering what the data means. Because there is no context for the data, it is difficult to translate it into actionable information that can drive improvement. Without context, team members cannot tell if the data indicates the desired performance or reflects a problem that should be investigated, and participants don’t know how it aligns with the facility’s progress toward achieving goals. Limiting QAPI to a monthly or quarterly meeting to report count data diminishes the scope and breadth of what QAPI is intended to accomplish. This article will define QAPI, provide a realistic example to demonstrate how it functions, and outline behaviors the nurse leader can model to exemplify QAPI use so that it becomes ingrained as the way to improve outcomes.
QAPI Defined
QAPI is a data-driven approach to improving the quality of all services offered by a facility, including quality of life and quality of care outcomes for residents. QAPI relies on systems thinking—a perspective that considers how various components influence one another as a whole, rather than looking at individual elements in isolation. QAPI tackles identified problems, such as underperforming quality measures or high staff turnover, but it also proactively seeks out weaknesses in systems before problems occur and initiates improvements to prevent poor outcomes.
QAPI is formed by merging reactive and proactive approaches. Both approaches are important to achieve the facility’s goals for high-quality care and services:
• QA, or quality assurance, is a reactive process focused on meeting quality standards and ensuring that care reaches an acceptable level. Staff in nursing facilities set thresholds to measure their compliance with regulatory requirements. QA examines why facility staff failed to meet certain standards and, using information learned, designs activities to improve quality and/or restore compliance. Frequently, however, once a problem is corrected, the efforts end. To address that lack of follow-through, CMS has clarified its expectation that staff will move beyond problem identification through the implementation of performance improvement (PI).
• PI is a proactive and continuous study of a facility’s processes with the intent of preventing or decreasing the likelihood that problems will occur. Opportunities for improvement are identified and new approaches are tried to correct the underlying causes of persistent or systemic problems. PI is used in nursing facilities to address residents’ quality of care and quality of life by not only correcting problems but also making the quality of care and quality of life even better (CMS, n.d.).
QAPI in Action
Because QAPI is data-driven, it’s necessary to understand some of the basic concepts used to translate data into actionable information.
- Goals – Measurable priorities for the department or the organization to achieve.
- Key Performance Indicator (KPI) – A measurable value that indicates if the things being done are working to accomplish the goals.
- Threshold – The minimum level of acceptable performance.
- Baseline – A measure of performance prior to an improvement being initiated.
The following scenario summarizes QAPI in action and provides a tangible example of how QAPI functions and benefits the facility. The concepts to translate data into information are woven throughout the scenario. Note that most of the activities to improve are done outside of the QAPI meeting.
Scenario
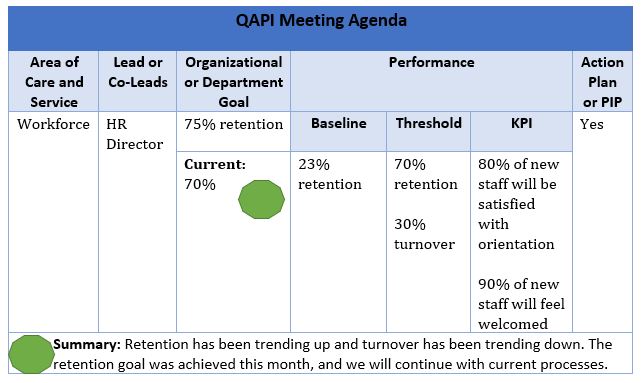
The facility’s QAPI Steering Committee or QAA Committee has identified that addressing high staff turnover is a priority and chartered a performance improvement project, or PIP. It sets a goal to achieve a staff retention of 75%, with a threshold of 30% turnover and provides this information to the PIP team. The PIP team, consisting of the Human Resource (HR) director as the lead, a certified nurse aide (CNA) from each shift, a charge nurse, and the DNS, works to determine the root causes and contributing factors of high turnover. After reviewing turnover rates, the PIP team learns that most turnover occurs within the first 60 days of employment. Therefore, they focus on further root cause analysis (RCA) for that time frame. Eighty percent of the turnover in the first 60 days is attributed to the following two root causes, which will be the priority areas to improve:
- New staff find orientation boring and they don’t retain most of the information they learn; orientation is limited to three days and is not individualized.
- New staff do not feel welcomed and integrated as valued members of the team; there is no formal structure for onboarding.
Knowing what processes to focus on, the PIP team engages in several Plan Do Study Act (PDSA) cycles to implement the improvements that will achieve and sustain the goal set by the QAPI Steering Committee. During the PIP and after, the QAPI Steering Committee discusses various data to determine if the goal for retention is being sustained and if the goal should be changed. The HR director presents the template below during the QAPI meeting, and provides an explanation of the PIP team’s work by translating the data into information.
HR Director states: The PIP team has fully implemented all new processes that directly relate to orientation and onboarding to improve retention. The goal to retain 75% of staff has almost been achieved this month, as you can see with the green light. We are trending in a positive direction for retention from our baseline of 23% and are at the threshold of 70%. We will continue to monitor our KPIs, which are that 80% of new staff will be satisfied with orientation and 90% of new staff will feel welcomed. We will also continue to monitor turnover to make sure we don’t go above the 30% threshold, as that could negatively impact our retention efforts. If we see our KPIs are declining or we cross the threshold, the PIP team will meet to determine what action needs to be taken.
High-Impact Leadership Behaviors
For QAPI to achieve its intended impact and become more than a meeting of department heads reporting count data, nurse leaders must continuously cultivate an environment in which all staff are valued as essential to improving care and services. In the above scenario, CNAs and a charge nurse were members of the PIP team because they bring a perspective that the HR director and DNS do not have but that will enrich the processes developed to achieve the goal. The Institute for Healthcare Improvement (IHI) identified five high-impact behaviors that leaders can emulate to promote improvement. It also identified actions the leader can engage in to demonstrate each behavior:
- Behavior 1 – Person-centeredness:
- Conduct rounds routinely and talk with staff, residents, and families.
- Include residents and families in the improvement.
- Explain outcomes in a way that illustrates how a person or people are impacted by the improvement.
- Make it public through word and deed that preventing harm and honoring resident choice is personally important and not mutually exclusive.
- Behavior 2 – Relationship-oriented:
- Develop relationships with the staff who work closest to the resident.
- Ask questions and learn what staff do and why they do it.
- Foster trust by being transparent.
- Demonstrate genuine concern for staff personally and recognize their contributions to the organization.
- Behavior 3 – Focus:
- Show a dedicated focus on where the organization is going and why.
- Spend time talking about the future.
- Take advantage of opportunities to share how what employees are doing contributes to achieving the goals.
- Share results and stories on a consistent basis that are associated with the goals.
- Appoint staff who are informal leaders to join an improvement team.
- Behavior 4 – Transparency:
- Share results and outcomes broadly; results should not be reserved for senior leaders only.
- Be honest and forthright when communicating.
- Behavior 5 – Boundarilessness:
- Look for connections at a systems level.
- Keep an open mind to new ideas, concepts, and ways of doing things.
- Look beyond the organization and even the industry for knowledge.
- Seek to understand the issues from multiple perspectives.
(IHI, 2017)
Summary
QAPI is a data-driven approach to improving the care and services that the facility provides. By engaging in the high-impact behaviors identified by the IHI and learning the data-driven quality improvement methodology fundamental to using QAPI, facility leaders will realize the full potential of QAPI in the form of achieving high performance that can be sustained.
References
Centers for Medicare & Medicaid Services. (n.d.). QAPI at a glance: A step by step guide to implementing quality assurance and performance improvement in your nursing home. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/QAPI/Downloads/QAPIAtaGlance.pdf
Institute for Healthcare Improvement. (2017, Jan. 10). High-impact leadership behaviors: Five things leaders can do to promote improvement. http://www.ihi.org/communities/blogs/high-impact-leadership-behaviors-five-things-leaders-can-do-to-promote-improvement
For permission to use or reproduce this article in full or in part, please complete a permissions form.
